Fertility medicine is a dynamic, living field of science. While clinical studies and testing can be a slow process, research is ongoing and new developments are being announced all the time. Many of these new discoveries may seem tiny, but all of these individual contributions from researchers add up to a formidable body of knowledge which is used to develop new treatments, technologies, and approaches to infertility. Any new piece of information can be the puzzle piece which leads to an important breakthrough.
All of us here at SCRC make it part of our mission to stay up to date with the latest news and cutting-edge research in our field, and we love passing on what we learn to our patients. Today, we’d like to share just a few on the most interesting fertility trends and advancements we’ve seen in the last year.
Trends in fertility and fertility treatment
Prevailing ideas and attitudes about infertility and the way we approach fertility treatment tend to shift and change over time. While the work we do is always focused on the particular needs of one unique patient at a time, it can sometimes be enlightening to take a wider perspective. Here are some recent fertility trends that have been making headlines recently.
A global fertility decline
Late last year, the National Center for Health Statistics (NCHS) released a report which examined how fertility rates in the United States have changed in the past decade. Covering a period from 2007 to 2017, this report found that total fertility rates had declined by 9% in rural counties, by 16% in small to medium metro counties, and by 18% in large metro areas. It also discovered that women are waiting longer before having babies. In rural areas, the mean maternal age increased by 1.3 years in rural areas, 1.5 years in small to medium areas, and 1.8 years in large metro counties. So people are having fewer children, and they are having them later in life.
These findings were echoed in a larger, global study, published in The Lancet, which looked at fertility rates from 1950 to 2017, covering 195 countries and territories throughout the world.
So what does this fertility decline mean for the average person who is thinking about their own fertility? Well, considering that many women may not be planning to even try for a baby until their mid-thirties, it is important to be informed and proactive about your fertility status early on. We know that women’s fertility tends to take a steep dive as their eggs age, which can lead to heartbreak when they are finally ready to conceive. As you are making your plans for the future, make sure you know your fertility options.
Fertility tests for younger women
Following on from the last item, we have been happy to see that routine fertility testing is becoming more common, even for younger women in their 20s and early 30s who might not have any pressing concerns about their fertility. You can get tested at any stage of your cycle, and even if you’re on hormonal birth control right now. An anti-mullerian hormone (AMH) blood test and ultrasound is enough to check on your ovarian reserve (the number of healthy eggs you still have). It’s a snapshot of your current fertility status, and an important data point when it comes to making decisions about when and whether you want to try for a baby, or whether you should think about freezing eggs for later. This new trend for early fertility tests is a very empowering shift: instead of waiting until there is a problem, young women are taking the reins and making sure they have the information they need to make informed choices about their futures.
Fertility preservation
It is an unfortunate fact of life that women’s age is one of the major limiting factors in fertility, but human nature often means that many people stay in denial about the realities of the human reproductive window until it is almost too late. As a technology, it’s the cause of so much stress, suffering, and expense, but it doesn’t have to be that way. Fertility preservation, or egg freezing, has been around for quite a long time, but elective egg freezing has only recently begun to gain popularity. This is another trend that we are very glad to welcome to the fertility landscape. Helped in part by more widespread information and education on the subject, as well as the face that the costs of egg freezing are falling, more and more women are choosing to freeze their eggs at earlier and earlier ages, effectively stopping the clock on their fertility until they are ready to get pregnant. While there’s never a guarantee in the world of medicine, fertility preservation offers more options and a chance to engage with your fertility on your terms.
New technologies for fertility treatment
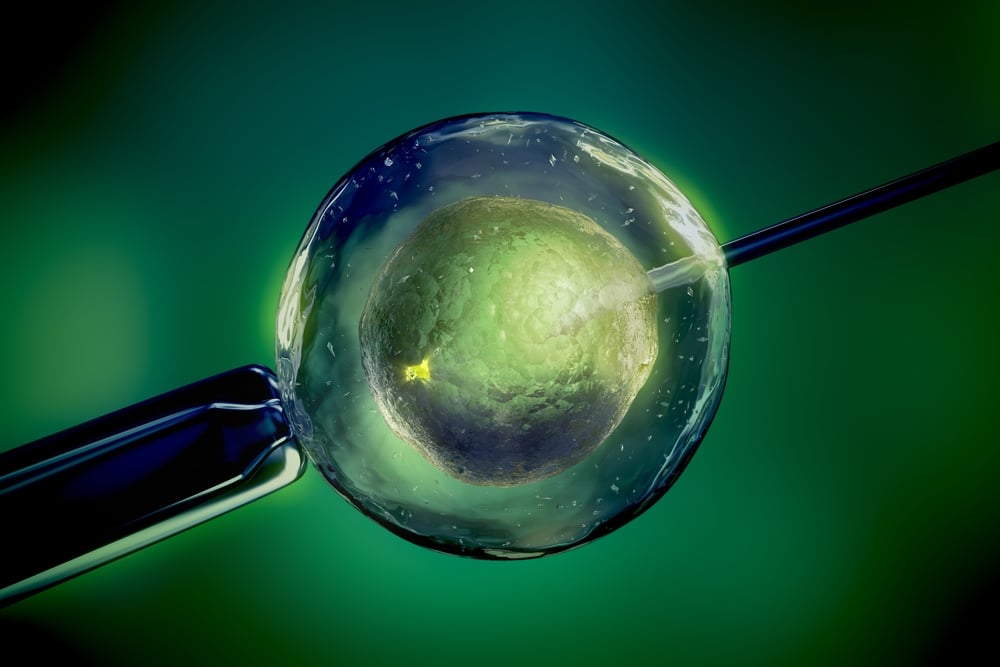
Technology is at the heart of almost everything we do as reproductive endocrinologists. It’s what allows us to offer our patients potentially life-changing, advanced fertility treatments like IVF. So we’re always excited to discover emerging technologies in the field which may end up revolutionizing the way we care for patients.
INVOcell
INVOcell was launched in 2016. The technology, which allows IVF-created embryos to be incubated in a device which is placed in the woman’s vagina before they are transferred to her uterus, has been introduced as a new development which may make IVF a more affordable option for more patients. It made the news in fall of 2018 for a truly joyful reason: using INVOcell, a lesbian couple made history by being the first same-sex couple to both physically participate in carrying their child. Bliss and Ashleigh Coulter, of Mountain Springs, Texas, decided to participate in reciprocal IVF, a popular fertility option for lesbian couples. The first part of the process began like traditional IVF: Bliss underwent ovarian stimulation and egg retrieval, and the resulting eggs were combined with donor sperm in the lab to create embryos. At this point, the embryos were then placed into an INVOcell device, which Bliss carried in her body for 5 days. At the end of the incubation period, the embryos were frozen, and eventually transferred to Ashleigh’s uterus. After a successful pregnancy, the couple are now the proud parents of a healthy baby boy.
Data analysis
Data analysis has always been an important part of fertility treatment, but as computers get faster and more powerful, our ability to spot helpful trends in huge data sets is growing. This is massively positive: in the near future, machine learning and artificial intelligence may have a lot to offer all branches of medicine, including fertility medicine. Some early advancements in this area are already changing lives. With the help of smarter data analysis strategies, so-called "precision medicine" is being used to help women suffering from repeated implantation failure. This is a particularly difficult situation, where patients undergoing IVF consistently fail to remain pregnant after the embryo transfer, even when all signs look positive and the embryos are of high quality.
The endometrial receptivity test is a fairly new test which can help us pinpoint her unique optimal time for conception so that we can schedule transfer on the day when her uterine lining is most receptive. This can end up improving her chances of getting and staying pregnant. The endometrial receptivity test looks at 238 genes in a sample of a woman’s endometrial tissue. When the endometrial (uterine) lining is receptive to implantation, the genetic material of these endometrial cells shows a unique expression, based on the amount of RNA generated by these cells. Using an extensive database containing more than 12,000 samples of endometrial tissue, researchers were able to determine the levels of RNA produced at different times of a woman’s cycle. Then, they applied advanced computer algorithms to the data set, searching for patterns which allow them to reliably classify a sample as "Receptive” or "Non-Receptive” according to its specific expression profiles. We are now able to use these findings to time embryo transfers, with great results.
Last year, fertility scientists in Estonia published new findings in the medical journal Human Reproduction, which may help make this test even more accurate and useful. The scientists measured the variability of cell shape and composition and how it relates to gene expression and receptivity in the endometrial tissue. This new approach offers a more specific method of gene expression profile analysis, which is exceptionally good news for patients. Here at SCRC, we’re actively involved in performing endometrial receptivity analysis (ERA) studies.
The next step in data analysis is finding new ways for artificial intelligence and machine learning to help us gain a more complete picture of how patients might respond to certain treatments. Algorithms are already being used in fertility treatment: the EmbryoScope software uses one to help the embryologist select the most viable embryos for transfer. Research continues as scientists work to develop self-improving AI algorithms which will continually update themselves as they encounter more data, offering us new insights and avenues for treatment.
More sophisticated embryo screening
Genetic screening of embryos has become an important option for many patients undergoing IVF. Pre-implantation Genetic Testing (PGT) has made it possible to screen embryos for a wide range of genetic diseases and disorders before they are potentially transferred to the uterus. Recently, it has also been used for sex selection of embryos. In November 2018, the New Scientist magazine reported that a company called Genomic Prediction has developed new genetic tests which can identify more specific potential traits in embryos. This new “polygenic testing” looks at traits which involve more than one gene, including heart disease, breast cancer, type 1 and type 2 diabetes, inflammatory bowel disease, and even intelligence levels. There are some serious ethical debates to be had about this level of screening, but from a pure science perspective, this is a very important advancement. In the future, rather than being used as a screening tool, this kind of testing may make it possible to perform gene therapy and repair on embryos.
Promising fertility research findings
Some of the most exciting recent fertility news relates to breakthrough research, conducted by dedicated scientists around the world. Some of the results and findings published in medical journals may still be years away from practical application to infertility treatments, but they give us all hope for the future.
Lab-grown eggs
One historic breakthrough in 2018 was something called in vitro gametogenesis: in short, lab grown eggs. A research team including scientists from Edinburgh University, the Royal Hospital for Sick Children, Edinburgh, and the New York Center for Human Reproduction reported their landmark achievement in the journal Molecular Human Reproduction. These researchers managed to develop human eggs to full maturity in the lab, outside of the human body, using ovarian tissue samples donated by ten women during c-sections. We know that for many women coping with reduced ovarian function or diminished ovarian reserve, the use of donor eggs in IVF can offer them exceptional success rates. The current reality, however, is that some patients feel a lot of ambivalence about using donor eggs. It may be quite some time before this breakthrough translates into real-world applications, but the potential is incredible. It may eventually offer a way to effectively “reverse infertility” for thousands of women across the world, allowing them to conceive and carry a baby who shares their full genetic heritage, even if they are unable to produce healthy eggs on their own.
DHEA treatment
Researchers at the University of Edinburgh published a breakthrough study in Fertility and Sterility in 2018 concerning the use of the fertility hormone DHEA. Their work found that using this hormone as a treatment could improve the receptivity of older women’s uteruses, giving them a better chance of successful implantation. Older fertility patients sometimes struggle with recurrent implantation failure and higher miscarriage rates. There are many possible reasons for this, but it is suspected that changes in the way the body produces the uterine lining may be involved. Usually, the uterus releases hormones during the menstrual cycle which signal the increased production of protein in the endometrial lining in order to create a receptive environment for the embryo and making it easier for implantation to occur. As a woman ages, the levels of these proteins may fall, leading to lower chances of implantation and pregnancy.
The researchers worked with donated healthy uterine tissue from women in their 40s who were undergoing unrelated surgeries. When they treated this tissue with DHEA, the scientists discovered that certain protein levels associated with successful and healthy implantation doubled. The also discovered that active androgens in the DHEA tissue also increased, providing a valuable clue that androgens may also have an important role to play in uterine receptivity. These findings have the potential to boost IVF success rates for women over the age of 40: a very exciting prospect.
Polarized light
In an exciting presentation at the 34th European Society of Human Reproduction and Embryology in Barcelona in 2018, a scientist from Australia presented new research which could have the potential to immediately improve the way IVF labs evaluate egg quality. Using a non-invasive polarized light technique to examine eggs in the lab during the ICSI procedure, the researchers discovered that the shape and profile of the oocytes (known as meiotic spindle morphology) could be used as a “predictive marker of fertilisation, blastocyst formation and the genetic normality of the resulting day 5 embryo.” This means that there may now be a relatively simple way to identify the eggs most likely to develop into viable blastocysts once fertilized.
More information of this type is extremely helpful to embryologists and may help improve the success rates of IVF. These are only some of the interesting new developments in the field. Things are ever changing, and we are excited to see what more comes along.